 People with a family history of type 1 diabetes can now conveniently participate in free screening to help find ways to delay or prevent the disease, even if they live far from a study site. This alternative to site-based initial screening comes as modern technology enables more secure online registration for medical research.
People with a family history of type 1 diabetes can now conveniently participate in free screening to help find ways to delay or prevent the disease, even if they live far from a study site. This alternative to site-based initial screening comes as modern technology enables more secure online registration for medical research.
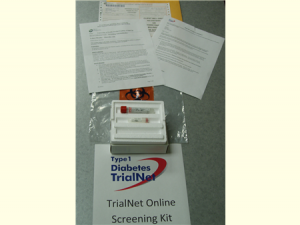
After volunteers consent online to participate in Type 1 Diabetes TrialNet — a study aimed at discovering ways to delay or prevent type 1 diabetes – they receive a screening kit in the mail, as shown, and will be directed to a local lab for a blood test at no cost to the volunteer. Courtesy of University of South Florida.
The screening, consisting of a questionnaire and blood test, is for Type 1 Diabetes TrialNet, a National Institutes of Health-funded long-term international collaboration. The collaboration is aimed at discovering ways to delay or prevent type 1diabetes in people at increased risk. TrialNet must screen more than 20,000 relatives of people with type 1 diabetes each year to perform studies to reach its research goals.
Previously, relatives needed to visit a study site or attend a screening event. But now, after answering a few questions online, eligible volunteers will receive a kit and be directed to a local lab for screening at no cost to the volunteer.
People who have antibodies associated with the development of type 1 diabetes will be contacted by a TrialNet center to review the results. They may be invited to have more blood tests at a study center, and may be invited to join a study aimed at preventing or delaying the disease. Children under 18 years old who do not have the antibodies can be retested annually to see if their risk has changed. Of every 100 people tested, typically only 3 or 4 will have antibodies showing an increased risk for type 1 diabetes.
“By ensuring the safety of people’s personal information while also making it easier to participate in clinical trials, we hope to find more people who are at risk and want to help find ways to delay or prevent type 1 diabetes,” said TrialNet Program Director Ellen Leschek, M.D., of the NIH’s National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), which oversees the trial.
Type 1 diabetes, once called juvenile diabetes, develops when the body’s immune system mistakenly destroys the insulin-producing beta cells of the pancreas. Insulin, a hormone, is needed to convert glucose (sugar) into energy. People with type 1 diabetes need insulin by daily injections or a pump to survive. However, replacing insulin is not a cure, and the disease may eventually damage the eyes, nerves, kidneys, and blood vessels. In adults, type 1 diabetes accounts for about 5 percent of the approximately 19 million people diagnosed with diabetes. Type 1 diabetes is not associated with obesity.
TrialNet studies have already helped. People at risk for type 1 diabetes who participated in TrialNet’s Pathway to Prevention Study were more likely to be diagnosed early.
“For people with type 1 diabetes, the importance of early diagnosis cannot be overstated,” said NIDDK Director Griffin P. Rodgers, M.D. “Early diagnosis means people are less likely to develop diabetic ketoacidosis, a life-threatening condition. Early diagnosis also means people can often control their diabetes more quickly, which may slow the loss of insulin-producing cells and may delay complications.”
Launched in 2001, TrialNet has also demonstrated that two drugs, Rituximab and Abatacept, slow the loss of insulin production in people with new-onset type 1 diabetes. This finding could improve diabetes control and delay complications. TrialNet has also contributed to research showing that anti-CD3, an immunosuppressive drug, can slow loss of insulin production. Three prevention studies are ongoing.
TrialNet is a network of 18 clinical centers working in cooperation with more than 200 sites throughout the United States, Canada, Finland, Britain, Italy, Germany, Australia and New Zealand. TrialNet is funded by NIDDK and other NIH components, including the National Institute of Allergy and Infectious Diseases and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, as well as the Juvenile Diabetes Research Foundation and American Diabetes Association.
Leave a Reply