 People with a family history of type 1 diabetes can now conveniently participate in free screening to help find ways to delay or prevent the disease, even if they live far from a study site. This alternative to site-based initial screening comes as modern technology enables more secure online registration for medical research.
People with a family history of type 1 diabetes can now conveniently participate in free screening to help find ways to delay or prevent the disease, even if they live far from a study site. This alternative to site-based initial screening comes as modern technology enables more secure online registration for medical research.
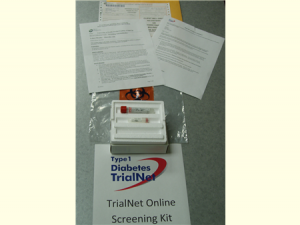
After volunteers consent online to participate in Type 1 Diabetes TrialNet — a study aimed at discovering ways to delay or prevent type 1 diabetes – they receive a screening kit in the mail, as shown, and will be directed to a local lab for a blood test at no cost to the volunteer. Courtesy of University of South Florida. [Read more…]